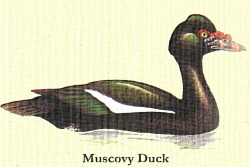
 Top Prize in the recent busting homeopathy stakes undoubtedly goes to Simon Singh for his wonderfully effective puncturing and deflating of the pompous David Tredinnick MP on the Today programme. Tredders was wind-bagging on about how they do homeopathy better in France, but he hadn’t bargained on Singh doing his homework. The best selling homeopathic remedy in France, said Singh, is a ’flu remedy made from the mashed up entrails of a single Muscovy duck that generates a staggering $15 million of revenue. It was, said Singh brilliantly, ‘the ultimate quack remedy’. Tredders had more than his wings clipped: he was permanently grounded; while Humph was reduced to muttering something about getting his hands on ‘that duck’.
Top Prize in the recent busting homeopathy stakes undoubtedly goes to Simon Singh for his wonderfully effective puncturing and deflating of the pompous David Tredinnick MP on the Today programme. Tredders was wind-bagging on about how they do homeopathy better in France, but he hadn’t bargained on Singh doing his homework. The best selling homeopathic remedy in France, said Singh, is a ’flu remedy made from the mashed up entrails of a single Muscovy duck that generates a staggering $15 million of revenue. It was, said Singh brilliantly, ‘the ultimate quack remedy’. Tredders had more than his wings clipped: he was permanently grounded; while Humph was reduced to muttering something about getting his hands on ‘that duck’.
Meanwhile, the BMA’s annual meeting had declared open season on homeopaths. Homeopathy, screeched one doctor, was ‘nonsense on stilts’. There were fervent calls to ‘strike a blow for science’ and to ‘protect our patients from this insidious practice’; and votes for the banning of homeopathic remedies from the NHS and pharmacy medicine shelves. Homeopathy wasn’t just having a bad hair day, it was having a shocking hair day.
While homeopaths might need something more potent than one of their remedies to get their hair back in order, the burst of quack-busting has nonetheless sparked some interesting debate on the relationship between homeopathy and the placebo effect, and so on to that most intriguing question: what exactly is the placebo effect?
Conventional wisdom is that the placebo effect is linked to the pill, but Margaret McCartney begs to differ, saying instead that the placebo effect arises from ‘caring effects’ – in other words, listening to people and looking after them properly – and the caring effect alone. The pill, she suggests, is a red (or blue or white or whatever) herring. “Using a ‘placebo tablet’ isn’t necessary to get ‘caring effects’,” she writes; the problem is not so much how to mimic the placebo effect of the homeopath by doling out a dummy pill as how to foster ‘caring effects’ in a target driven, outcomes focused NHS. NorthernDoctor (and others) reckon McCartney is ‘spot on’ – and the NorthernDoctor goes even further: in a post of his own he extends the idea that the placebo effect is greatly over-rated.
Dr No agrees that the NHS does little to foster (and may actively antagonise) ‘caring effects’, but is far from persuaded that the placebo effect is merely a ‘caring effect’ that does not need a pill to achieve its effect. It seems to him that we may be confusing ‘caring effects’ – active listening, the ordinary laying on of hands, showing that ‘we care’ – ie human activities – with ‘treatment effects’, where something said to be therapeutic is done or given to the patient.
The etymology is illuminating. Although McCartney redefines placebo as ‘caring effects’, the word in fact comes from the Latin placebo, meaning ‘I shall please’. The focus is not so much on caring for the patient (important as that is) as on pleasing the patient – giving him or her something he or she values and wants because it has been invested with therapeutic potential. Dr No has little doubt that that wonderful thing we call the human mind is more than capable of turning an expectation of benefit into actual benefit; and so of harnessing benefit from both being cared for and being pleased.
Indeed, support for the separate existence of a placebo effect in its own right comes from studies that have manipulated simple physical characteristics of placebos to determine what effect, if any, these characteristics have on the placebo effect. Not only does colour affect response (calming colours such as blue and green are more sedative than invigorating colours like red), so too do form (capsules beat pills) and quantity (more pills more often is best). These factors – colour, form and quantity – are inherent to the placebo – and as such are independent of any caring effects – and simply could not happen were the placebo effect were solely due to caring effects.
Even the great evidence based Cochrane Collaboration now grudgingly admits that the placebo effect exists – even if they do their best to play it down. Although the normally meticulous NorthernDoctor quotes the Collaboration as saying:
‘There was no evidence that placebo interventions in general have clinically important effects. A possible small effect on continuous patient-reported outcomes, especially pain, could not be clearly distinguished from bias.’
this in fact comes from an earlier (2006), more disparaging, review, while the most recent (2009) review reports mostly significant overall pooled effect estimates (albeit not large, and possibly biased, but nonetheless significant) and concludes:
‘We did not find that placebo interventions have important clinical effects in general. However, in certain settings placebo interventions can influence patient-reported outcomes, especially pain and nausea, though it is difficult to distinguish patient-reported effects of placebo from biased reporting.’
Note the subtle shift in emphasis from ‘no evidence’ to not finding evidence of ‘important’ clinical effects – which is of course another way of saying we did find evidence of effect – but consider it trivial.
While the evidence based medicine hard-nuts at the Collaboration may choke at having to admit it, it does seem clear that there is evidence for a separate placebo effect that can and does exist of and by itself alongside McCartney’s ‘caring effects’. Dr No is comfortable with this: as a somewhat Balint minded doctor, he believes that not only do we need to study – and make use of – the pharmacology of the drug ‘doctor’ – in other words, McCartney’s ‘caring effects’ – but also that of the placebo. Only then will we be in a better position to harness the twin benefits of these remarkable effects. And – who knows – one day we might even be able to tease out whether that homeopathic ’flu treatment really is – as Dr No is inclined to suspect will turn out to be the case – all quack and no bang – and so really is the ultimate quack remedy.
