 There’s not much to say, even if Dr No is going to say a bit, about Atul Gawande’s third 2014 Reith Lecture, except that he blew it in the title – overweening confidence, Gawande’s definition of hubris, is not the problem, striving officiously in hopeless desperation is – and then spent thirty or so minutes stating the bleeding obvious. Called The Problem of Hubris, the lecture dealt with doctors’ failure to deal with the inevitable, the appointment we all must keep when our bell tolls, the appointment not with a doctor, but with death.
There’s not much to say, even if Dr No is going to say a bit, about Atul Gawande’s third 2014 Reith Lecture, except that he blew it in the title – overweening confidence, Gawande’s definition of hubris, is not the problem, striving officiously in hopeless desperation is – and then spent thirty or so minutes stating the bleeding obvious. Called The Problem of Hubris, the lecture dealt with doctors’ failure to deal with the inevitable, the appointment we all must keep when our bell tolls, the appointment not with a doctor, but with death.
Time for a Gawande anecdote, this time about a friend called Peg. Emotional strings were taughtened by casting Peg as piano teacher to Gawande’s 13 year old daughter. Given Gawande’s subject, one knew Peg’s cards were marked: at some point, Peg would peg out. Best be grateful for small mercies: at least Peg wasn’t called Sue. Peg had a recurrent sarcoma, a nasty tumour, and had already endured heroic treatment, complications and yet more heroic treatment. Peg, her family, her doctors and Gawande faced a dilemma: ever more extreme treatment of increasing dubiousness in a heroic fantasy, or letting go? Facing the dilemma, Gawande felt troubled. Neither option felt right. Where, he asked, was the missing third way? Heroics – striving officiously – could only make Peg worse, but letting go felt like giving up.
So he asked a lot of people – he lost count of how many – and discovered, or rather was reminded, as medicine has known this for some time, even if it often forgets it, that its practise is not just about adding time to life – something it has done rather well over the last half century, but adding life to time. And as we approach the end, the balance for each of us is different. Three good months rather than twelve bad months for one; for another, twelve tolerable months to reach an important event – a wedding, or the chance to see a new grandchild.
We all have our priorities, and heads down no nonsense mindless extension of life whatever the cost is rarely, if ever, the only one. So we need to ask patients what their priorities are, in all the circs. This doesn’t mean crashing about with facts and figures, for often there are none, only probabilities, often vague, and as Dr No is wont to say, prognosis is the original piece of string whose length is not known until it is cut. Instead, it involves sensitive open-ended questions that allow the patient to develop and express what matters to them. For Dr No’s mother – Dr No is not above the family anecdote stunt either – it was dying at home. This mattered far more to her than how long her piece of string was. The necessary steps were taken, and her goal was achieved, though not without a few bumps along the way. It wasn’t a good death – there is no such thing as a good death, though some might be merciful, others peaceful – but it was a less bad death than the hospital one she dreaded.
Much the same happened to Peg, and she was also able to do what mattered to her. She ditched the curative treatment, managed to do some music teaching that included four sessions with Gawande’s daughter, and pegged out at home some six weeks later. Gawande presented much of his lecture as if it was something new from a book of revelations. Perhaps it is to American surgeons, but to British medicine it is not. We have known these principles for decades; the tragedy is we all too often fail to apply them.
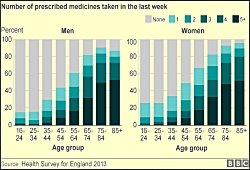
Elsewhere, news emerged that almost half of all English adults are popping pills. The numbers by age – see the graph above – are not unlike the prevalence of prostate cancer in men: the percentage of pill poppers roughly mirrors age. If this isn’t striving officiously on a population scale, then Dr No doesn’t know what is. On hand was Hugh Pym, the BBC’s answer to Horlicks in human form, to tell us about it. Far from being horrified, Hugh mused. Was there a pill for every ill, he wondered? And yet… are we popping too many pills, he mused? Could the costs get out of control, he pondered? On the other hand, he put it to us that the total bill for drug costs in England last year in some ways sounds reasonable, or something along those lines. Perhaps we should all get fitter, and ditch the pills? There was a lot to be mused over. It was all very perplexing. The Horlicks helped keep things calm. It’s hard to be horrified when you are sipping Horlicks. As Dr No drifted off, Hugh’s only one and single clichéd answer swirled round his mind: there are no easy answers. Then something snapped, Dr No put down his Horlicks, and thought: but there are. In fact there is only one, and it’s the same for both Gawande’s hubris and Hugh’s pill poppers, because they are different aspects of the same problem: over-medicalisation. The answer? We need to stop medicalising the normal.
